Navigating your brain's health and mental well-being can feel complex. Understanding the difference between neurology vs psychiatry is a helpful and empowering first step on your journey.
Think of it this way: neurology deals with the physical "hardware"—your brain, spinal cord, and nerves. Neurologists address conditions like migraines, strokes, or multiple sclerosis. Psychiatry, on the other hand, focuses on the "software"—your mind, emotions, and thoughts—helping you manage challenges like anxiety, depression, or burnout.
Understanding the Core Difference Between Neurology and Psychiatry
When symptoms feel overwhelming, choosing between a neurologist and a psychiatrist can be a real challenge. Both are medical doctors who specialize in the brain, but they approach it from different angles to support your health and well-being. A helpful analogy is to think of a neurologist as an electrician for your body’s wiring, while a psychiatrist is an expert in the operating system that helps everything run smoothly.
This distinction is crucial for getting the right kind of support. Whether you're navigating workplace stress that affects your focus or experiencing physical symptoms causing you distress, knowing who to see first can make a significant difference.

The Brain Versus the Mind
The simplest way to understand the difference is to separate the physical brain from the mind. Your mind includes your thoughts, emotions, and experiences.
- Neurology is about the brain's physical structure and function. Neurologists are trained to find and treat diseases affecting the nervous system.
- Psychiatry focuses on your mental health, which includes your emotional landscape and behavioral patterns. Psychiatrists help you understand how your thoughts and feelings shape your daily life.
This fundamental difference guides their approach. A neurologist might order an MRI to look for a physical cause, while a psychiatrist may use therapy and counselling to help you build emotional resilience and compassion.
A neurologist asks, "What is physically happening in the brain and nervous system?" A psychiatrist asks, "How are your thoughts, feelings, and behaviours affecting your well-being?"
Both specialists are dedicated to helping you live a healthier, more fulfilling life. The table below outlines their distinct roles to make the comparison clear.
| Aspect | Neurology | Psychiatry |
|---|---|---|
| Primary Focus | The physical nervous system (brain, spine, nerves) | Mental, emotional, and behavioural health |
| Common Conditions | Epilepsy, stroke, migraines, Parkinson's disease | Depression, anxiety disorders, workplace stress, bipolar disorder |
| Key Approach | Diagnosing and treating structural or electrical issues | Understanding and improving thoughts, feelings, and coping mechanisms |
| Treatment Tools | Medication, physical therapies, diagnostic imaging (MRI/CT) | Psychotherapy (therapy), counselling, medication management |
The Different Paths of Neurologists and Psychiatrists
To truly grasp the neurology vs psychiatry distinction, it helps to look at how these specialists are trained, particularly in an India-first context. Both begin with an MBBS degree, but their paths diverge significantly from there. This specialized training shapes them into the distinct professionals they become and helps you decide who is the right fit for your health concerns.

This focused education ensures each doctor develops a deep, yet different, understanding of the brain. Their unique approaches are designed to address the separate challenges of the brain’s physical health versus our emotional and mental well-being.
The Neurologist’s Journey to Expertise
A future neurologist first completes an MD in General Medicine before pursuing a highly specialized DM in Neurology. This demanding training sharpens their skills in interpreting complex diagnostic tools like MRIs, CT scans, and EEGs. Their entire focus is on identifying and treating physical, structural, or electrical problems within the nervous system.
This path makes them the go-to experts for conditions where a problem can be traced to a physical cause. They are trained, for instance, to find the source of seizures or the anatomical reasons for chronic migraines.
The Psychiatrist’s Path to Understanding
A psychiatrist takes a different route, completing an MD in Psychiatry. Their training centers on understanding the mind from various perspectives, including psychotherapy, counselling techniques, and psychopharmacology—the science of how medication affects mental health. They learn to assess thought patterns, emotional distress, and behavioral health, making them experts in conditions like anxiety and depression.
This training difference is fundamental: one specialist becomes an expert in the brain’s physical framework, while the other becomes an expert in mental and emotional health, promoting resilience and overall well-being.
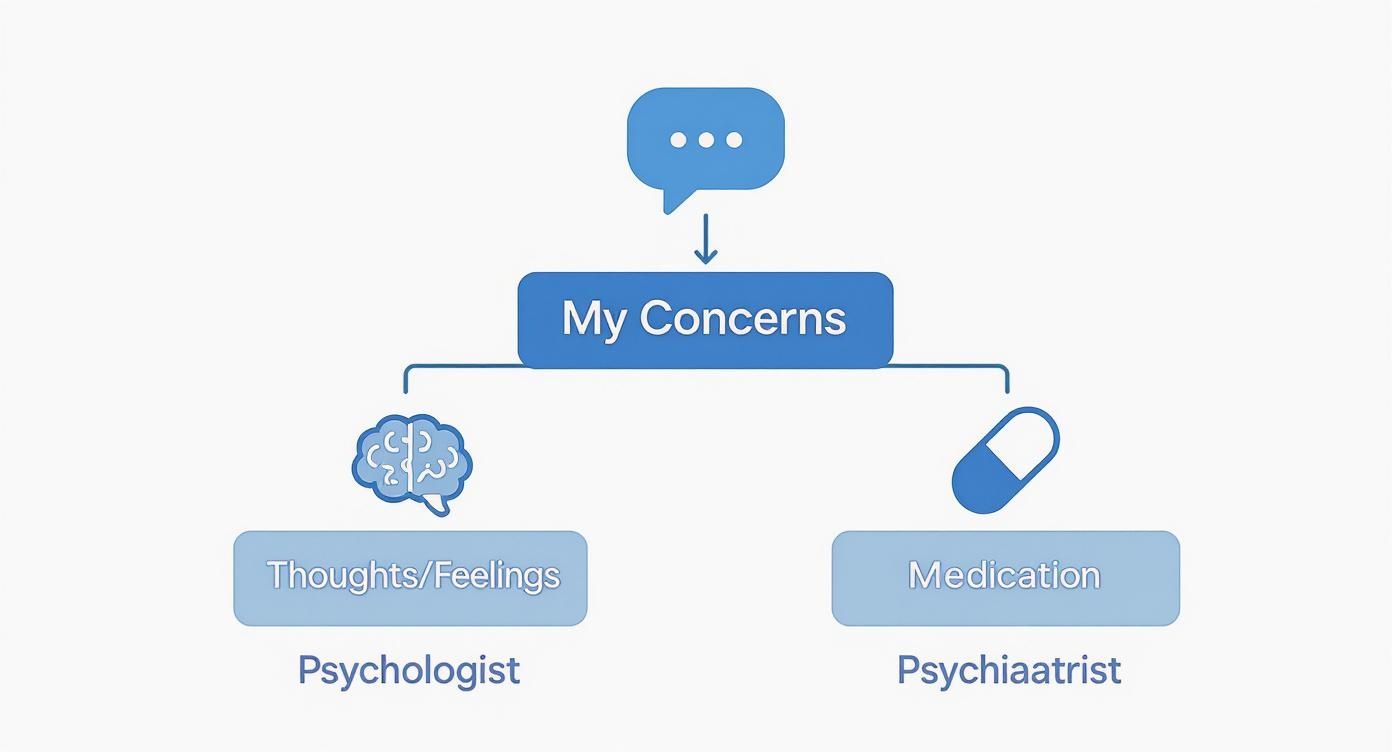
Their education equips them to guide people through challenges like workplace stress using tools like talk therapy and other supportive treatments. For a broader view, it can be helpful in understanding the distinctions between other mental health specialists, such as psychologists and psychiatrists. This knowledge helps ensure you find the right professional for your journey toward happiness and well-being.
A Practical Comparison of Neurology and Psychiatry
Knowing the definitions is one thing, but seeing how neurologists and psychiatrists work in the real world makes the difference clear. Their day-to-day approaches, from the conditions they treat to the tools they use, cut through the jargon. This practical perspective helps you figure out where your own health concerns might fit.
Let's explore how their methods differ when dealing with the intricate relationship between the brain and the mind. Looking at their work this way makes the choice between a specialist for a physical issue versus a mental or emotional one much simpler.
Focus of Care and Common Conditions
Think of a neurologist as a skilled mechanic for the body's electrical system. Their world revolves around the physical machinery of the nervous system. They are the experts for conditions with a clear, identifiable cause in the brain, spinal cord, or nerves.
- Neurological Conditions: This includes epilepsy, debilitating migraines, stroke, Parkinson's disease, and multiple sclerosis. Symptoms are often tangibly physical, like tremors, seizures, or persistent headaches.
A psychiatrist, in contrast, is focused on your mental and emotional landscape. They work with conditions affecting your thoughts, feelings, and behaviors that often don't appear on a brain scan. Their job is to understand your unique experience and support your well-being.
- Psychiatric Conditions: This area includes challenges like depression, generalized anxiety, bipolar disorder, and the heavy toll of workplace stress. The goal is not just to treat a symptom but to improve your mood, build coping skills like resilience, and enhance your overall quality of life.
Diagnostic Tools and Methods
The tools each specialist uses highlight their different approaches. A neurologist relies on technology that allows them to see the brain's structure and electrical activity, hunting for physical clues.
A neurologist uses objective tests to find physical evidence, while a psychiatrist uses conversation and observation to understand your inner experience.
In contrast, a psychiatrist's most powerful tool is conversation, often guided by structured assessments. Through therapy and counselling sessions, they listen to your personal history, explore your thought patterns, and gain a sense of your emotional state. While assessments are informational, not diagnostic, they help guide the conversation toward healing.
This difference also appears in patient experiences. A study in India found that health anxiety was more common among patients in psychiatric settings (25%) than in neurology clinics (19%). This highlights how psychiatry often addresses the emotional weight of health worries. You can read the full research about these findings to learn more.
Treatment Modalities
Once a direction is clear, the treatment paths also differ. Neurological treatments are typically aimed at managing or correcting a physical problem. This might involve medication to control seizures or therapies to help regain function after a stroke.
Psychiatric treatments are geared toward improving mental well-being and fostering resilience and compassion. A psychiatrist might suggest medication, like an antidepressant, to help with emotional balance. This is often part of a larger plan that includes psychotherapy or counselling, which are cornerstones of care that empower you with healthier coping strategies.
To make this even clearer, here's a quick side-by-side look.
At a Glance: Neurology vs Psychiatry
This table provides a clear, side-by-side summary of the key differences between a neurologist and a psychiatrist, helping you quickly identify the right specialist for your needs.
| Aspect | Neurologist | Psychiatrist |
|---|---|---|
| Area of Focus | The physical structure and function of the nervous system (brain, spinal cord, nerves). | Mental, emotional, and behavioural health; your thoughts and feelings. |
| Common Conditions | Epilepsy, stroke, migraines, Parkinson's disease, multiple sclerosis, dementia. | Depression, anxiety disorders, bipolar disorder, schizophrenia, PTSD, stress. |
| Diagnostic Approach | Physical exams, brain imaging (MRI, CT scans), EEG, lab tests to find a physical cause. | Clinical interviews, psychological assessments, conversation, observation, DSM-5 criteria. |
| Primary Treatments | Medications (e.g., anti-seizure drugs), physical therapy, surgical procedures, nerve blocks. | Psychotherapy (therapy), counselling, medications (e.g., antidepressants, mood stabilisers). |
| Patient Interaction | Focused on investigating physical symptoms, interpreting test results, and managing a specific disease. | Explores personal history, feelings, thought patterns, and building coping mechanisms. |
While both specialists work with the brain, their perspectives and methods are distinct. This ensures that you receive the right kind of care for your specific needs, whether that involves addressing physical challenges or nurturing your mental well-being.
Knowing When to See a Specialist
Sometimes, looking at real-life situations is the best way to understand the difference between neurology and psychiatry. These examples can help you see your own experiences more clearly and find the right support. The most important clue is often the nature of your main symptoms.
For instance, imagine a college student in Delhi with crippling headaches that disrupt their studies. Since headaches are a physical symptom, a neurologist is the right specialist to see first. Similarly, an older person experiencing memory loss along with tremors should see a neurologist to check for underlying physical conditions.
Navigating Emotional and Behavioural Challenges
Now, think of a young professional in Bengaluru feeling overwhelmed by workplace stress. They have a persistent low mood, have lost interest in hobbies, and struggle to concentrate, which are common signs of depression and anxiety. A psychiatrist or a therapist would be the best fit, offering counselling and support to build mental resilience.
This clear distinction can make the decision much easier. The decision tree below breaks it down further, helping you sort symptoms into physical or mental categories.
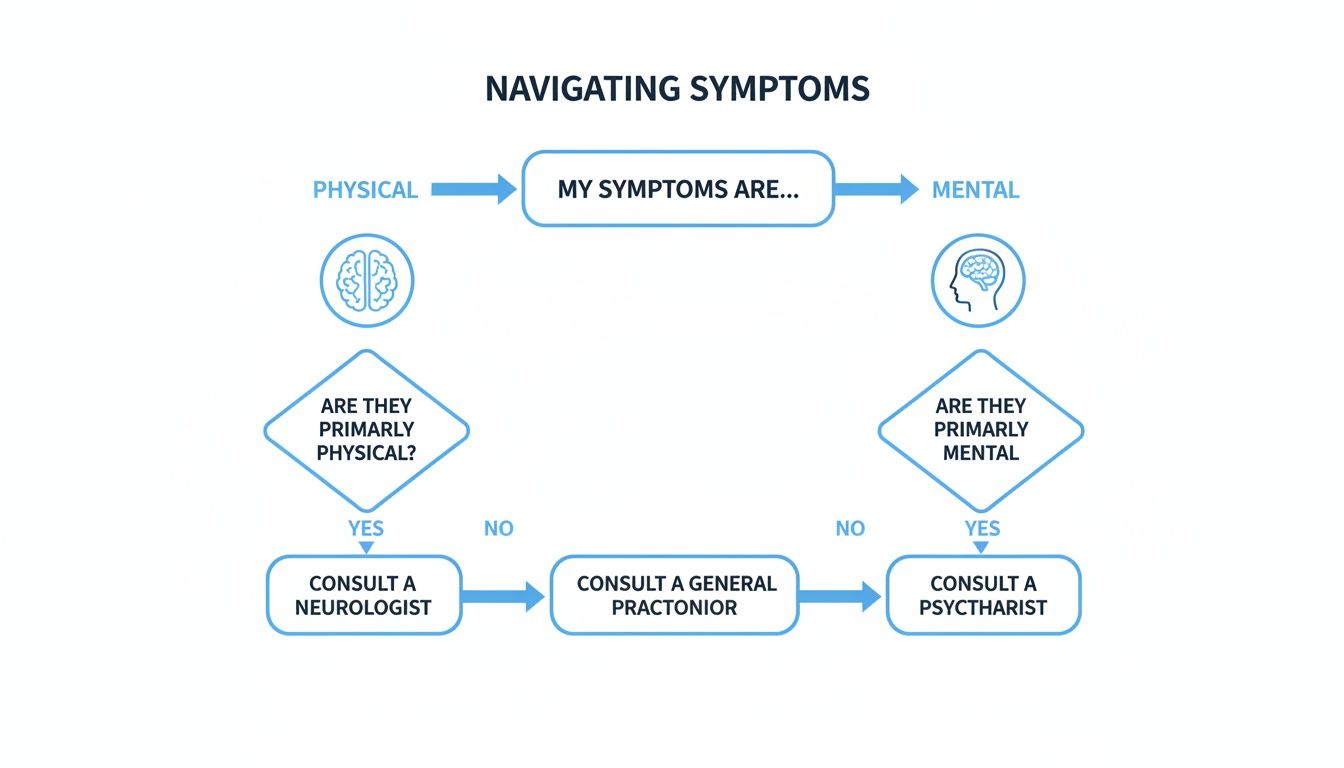
As the guide shows, if your main challenges are physical—like seizures, muscle weakness, or chronic pain—a neurologist is your go-to expert. If the symptoms are primarily emotional or behavioral, a psychiatrist or therapist is better equipped to help.
When Symptoms Overlap
Of course, life is rarely so neat, and many conditions blur the lines between neurology and psychiatry. For example, the depression that can accompany Parkinson's disease often requires a team approach. A neurologist manages the physical symptoms, while a psychiatrist provides therapy and support for the patient's mental well-being.
This overlap is a significant and growing health challenge in India and globally. The impact of neurological disorders has increased dramatically, highlighting the urgent need for integrated care where neurological treatment and mental health support go hand-in-hand.
Seeking support is a sign of strength. Whether your challenges feel physical or emotional, acknowledging them is the first step toward building resilience and reclaiming your well-being.
Assessments are always informational, not diagnostic, but they can bring much-needed clarity. If you need help knowing where to begin, resources on finding the right mental health professional can be very useful. Remember, you don’t have to figure this out alone; professional guidance is available to help you find your way.
Your First Step Toward Mental Well-Being
When you’re unsure if your symptoms are neurological or psychiatric, a good starting point is gentle self-reflection. This isn't about self-diagnosis but about taking a compassionate moment to understand what you're feeling. It's about gathering your thoughts before deciding on the next step.
Platforms like DeTalks can be very helpful here. They offer scientifically backed psychological assessments that are informational tools, helping you get a clearer picture of your emotional state. It's important to remember that these are not diagnostic tests; they are designed to help you spot patterns related to challenges like anxiety, workplace stress, or depression.
The insights from these assessments can offer a sense of direction. They might suggest that starting counselling or therapy is a good idea or that consulting a medical specialist is the next best step. It's a gentle, supportive way to begin your journey toward greater well-being.
Building Resilience and Seeking Support
Understanding your emotional health is the first step toward building resilience. Life can bring many challenges, sometimes leading to burnout or a persistent sadness. Acknowledging these feelings is a sign of strength, not a weakness.
Tools like self-assessments can help you articulate what you're feeling, making the process feel less overwhelming. They offer a private and accessible way to start exploring your mental health. This is especially important in a country like India, where access to care can vary widely.
For example, a landmark survey in Bangalore found that neurological disorders were twice as common in rural areas as in urban ones. This difference underscores how vital accessible platforms are in bridging the care gap. You can discover more insights about these neurological care disparities to see why initial guidance is so critical.
Your Compassionate Path Forward
Taking that first step, whether it's an assessment or talking to someone you trust, is a powerful move toward positive change. The goal is to feel empowered, not overwhelmed, by your health journey.
Remember, the purpose of any assessment is to provide insight, not a label. It is a tool to help you start a conversation, either with yourself or a professional, about your well-being.
Everyone's journey is unique, and finding the right support is a personal process of discovery. Whether your path leads to counselling for anxiety, therapy to build resilience, or a medical consultation, every step is progress. The aim is to find balance, happiness, and a renewed sense of purpose.
Frequently Asked Questions
It's completely normal to have questions when trying to understand your brain and mind. Here are some clear, simple answers to common queries to help you on your way.
Can a Neurologist Treat Anxiety or Depression?
A neurologist does not directly treat anxiety or depression. Their role is to determine if these feelings might be symptoms of an underlying neurological issue, such as a brain injury or a specific disorder.
If they rule out a physical cause, they will refer you to a psychiatrist or therapist. These professionals provide the right kind of care, like counselling and therapy, to support your mental and emotional health.
Do I Need a Referral to See a Specialist in India?
In India, you can often book an appointment directly with a neurologist or psychiatrist. However, starting with your General Practitioner (GP) is usually a good idea.
Your GP can conduct an initial check-up and help you decide which specialist is the best fit for your symptoms. This can save you time and ensure you connect with the right expert from the start.
Clarifying the First Step: Think of your GP as your first point of contact. They can help make sense of your initial symptoms and direct you to the specialised neurological or psychiatric care you actually need.
What If My Symptoms Are Both Physical and Emotional?
This is very common because the mind-body connection is strong. For example, chronic pain from a neurological condition can lead to depression. Similarly, severe anxiety can cause physical symptoms like headaches or stomach issues.
When symptoms overlap, a team-based approach is best. Your GP can help coordinate care between a neurologist for the physical symptoms and a psychiatrist for your emotional well-being. This creates a complete, supportive treatment plan.
How Do I Know If Memory Loss Is Neurological or Psychiatric?
Memory loss can be complex as it can stem from both physical and emotional causes. A neurologist may use brain scans like an MRI to look for physical changes linked to conditions like Alzheimer's disease.
A psychiatrist, on the other hand, will explore if memory issues are related to challenges like severe depression, trauma, or chronic stress. A professional evaluation is essential to determine the root cause and find the most supportive takeaways for your situation.
Getting clear answers is the first step toward feeling better. DeTalks provides confidential, science-backed assessments that can help you understand your emotional well-being and connect you with the right professionals for therapy or counselling. Start exploring your path forward at https://detalks.com.