Deciding between a counsellor and a psychologist comes down to their training and the kind of support they offer. A psychologist often has advanced education, including formal assessments, preparing them to help with persistent mental health conditions. A counsellor typically uses talk therapy to help you navigate specific life challenges, like workplace stress or grief.
Navigating Your Path to Mental Well-being

Taking the first step to seek support is an act of strength. It can also feel confusing, as terms like 'counsellor' and 'psychologist' are often used interchangeably. Understanding the difference is key to finding the professional who best aligns with your personal journey.
This guide is here to bring clarity and help you choose with confidence. It’s not about which professional is “better,” but about finding the right fit for your unique needs and goals for your well-being. We'll explore their education, the concerns they handle, and how their approaches to therapy can differ.
Counselor vs Psychologist at a Glance
To start, here is a simple summary of the key differences between these two mental health professionals. This can help you understand their primary distinctions.
| Aspect | Counselor | Psychologist |
|---|---|---|
| Primary Focus | Addresses specific life challenges, like workplace stress or relationship issues, through supportive talk therapy. | Works with a range of mental health concerns, from anxiety and depression to more complex conditions. |
| Approach | Goal-oriented and supportive, focusing on building coping strategies for improved emotional well-being and resilience. | May use a combination of therapy, psychological assessments, and structured treatment plans. |
| Education | Typically holds a Master’s degree in counselling or a related field, with a focus on therapeutic techniques. | Holds advanced degrees (Master's, M.Phil, or Doctorate) with extensive training in human behaviour and psychological theory. |
| Assessments | Generally does not conduct formal psychological testing; these assessments are informational, not diagnostic. | Trained and often licensed to perform psychological assessments to help inform the therapy process. |
This table provides a quick overview, but the details are what will help you find the right support. Both professionals are dedicated to helping you build resilience, find compassion, and lead a more fulfilling life.
Why This Distinction Matters for You
Understanding these roles empowers you to choose a path that feels right from the start. This ensures your journey to well-being begins on a solid foundation of understanding and trust.
Are you looking for practical guidance to navigate a period of burnout or build more happiness in your life? A counsellor could be an excellent partner for that journey. Their focus on therapy and practical skills can help you build resilience and compassion.
However, if you're dealing with persistent feelings of anxiety or depression that impact your daily life, a psychologist’s expertise might be a better fit. They are trained to explore the deeper patterns of thought and behaviour that may be holding you back.
Comparing Education, Training, and Licensure
One of the clearest ways to understand the difference between a counsellor and a psychologist is by looking at their education. Their training paths are quite different, shaping their skills and the kind of support they can offer. This foundational training builds trust and clarifies why their roles are distinct yet equally important for your mental well-being.
A counsellor’s education focuses on building strong therapeutic and supportive skills. In India, this usually means a Master’s degree in counselling or psychology. Their training emphasizes talk therapy techniques and creating a safe space to work through life’s challenges.
The goal is to prepare them to help with common issues like workplace stress, relationship problems, or grief. Their education shapes them into empathetic guides who can help you build resilience and find practical ways to move forward.
The Psychologist’s Rigorous Path
The journey to become a clinical psychologist in India is more intensive and specialised. It typically requires an M.Phil in Clinical Psychology, a demanding two-year training program. This advanced qualification is essential for licensure by the Rehabilitation Council of India (RCI).
This process involves deep training in psychological theories, research, and administering psychological assessments. These assessments are informational tools that help create a clearer picture of what might be causing challenges like severe anxiety or depression. They are not about assigning labels.
The RCI license is a crucial differentiator. It signifies that a professional has met a high standard of training, allowing them to work with a broader spectrum of mental health concerns and conduct formal psychological evaluations.
Why Licensure and Regulation Matter
In India, these educational requirements create a clear distinction between counsellors and psychologists. Counsellors, with their Master's degree, are well-qualified for many support roles without a specific license for formal diagnosis. Psychologists, however, must complete an RCI-approved M.Phil to practice clinically.
The RCI, established in 1993, is the regulatory body. As of 2023, there were only about 4,200 RCI-licensed clinical psychologists in India, compared to over 50,000 counsellors. You can find out more about how these paths shape psychologist salaries and career trajectories in India.
This distinction ensures that professionals who handle more complex mental health conditions have standardised training. While counsellors are skilled at providing therapy and support for personal growth, the RCI license gives psychologists a specific scope of practice that includes formal assessment. To learn more about different roles, a guide to the Top 10 Roles in Mental Health Careers can provide excellent context.
Global Perspectives on Training
While the RCI framework is specific to India, this difference in training is consistent globally. In countries like the USA or the UK, psychologists also complete more extensive doctoral-level education and must be licensed to practice. Counsellors in these regions also require a Master’s degree and a license but focus on therapeutic counselling.
Both paths create dedicated professionals committed to supporting mental health. Understanding their training helps you appreciate their unique strengths, ensuring you find the right expertise for your needs.
Exploring Their Scope of Practice and Therapeutic Approaches
To truly understand the difference between a counsellor and a psychologist, it’s helpful to look at what they do in a session. Their scope of practice is a direct result of their training and dictates the kind of support they are best suited to provide. This knowledge helps you connect with the right professional, whether you're looking to build resilience or work through deeper mental health concerns.
A clinical psychologist's role is often more structured. They are trained to use formal psychological assessments to better understand patterns behind conditions like major depression, severe anxiety, or trauma. These assessments are informational tools, not labels. They help create an effective, personalised therapy plan aligned with your unique situation.

A Counsellor’s Focus on Guidance and Well-being
A counsellor’s work is centered on providing guidance, support, and a safe space to explore life challenges. Their primary tool is talk therapy, a collaborative conversation where you can speak freely. They help you develop practical coping strategies for issues like workplace stress, relationship hurdles, or grief.
Their approach is typically goal-oriented, focusing on your present situation and empowering you with self-awareness and skills. The goal is to foster personal growth, a better sense of well-being, and stronger resilience.
In India, the scope is quite defined: psychologists are authorised for formal diagnosis and therapy, while counsellors primarily offer guidance. This specialisation affects session fees, and you can learn more about how this impacts psychology-related careers and salaries in India.
Therapeutic Approaches: A Side-by-Side Look
The methods used by counsellors and psychologists often reflect their distinct training. While both may use similar talk therapy techniques, the application and depth can vary.
Here’s a simple way to think about their common therapeutic approaches:
- A Counsellor often uses:
- Client-centred methods like Person-Centred Therapy, where you guide the conversation in a supportive, non-judgmental space.
- Solution-Focused Brief Therapy (SFBT) to help you identify your strengths and find practical solutions for immediate problems, like managing burnout.
- A Psychologist may employ:
- Specialised therapies like Cognitive Behavioural Therapy (CBT), an effective approach for anxiety and depression that helps change unhelpful thought patterns.
- For more complex issues, they might use psychodynamic therapy to explore how past experiences shape the present or other evidence-based treatments.
Key Takeaway: A counsellor's approach often focuses on improving your well-being and managing life's stressors. A psychologist's toolkit is built to handle both life challenges and more complex mental health conditions.
Real-World Scenarios: Making the Choice Clearer
Let’s bring this to life with a couple of common situations.
Scenario 1: Dealing with Workplace Stress
Anjali feels overwhelmed by constant pressure at her job, leading to burnout and a loss of happiness. She needs practical strategies to manage her workload and set boundaries. In this case, a counsellor would be an excellent choice to provide the guidance and support she needs to navigate workplace stress.
Scenario 2: Persistent Feelings of Sadness
Rohan has been experiencing a deep sadness for months, affecting his sleep, relationships, and enjoyment of life. A psychologist would be better suited to help him explore the root causes of his feelings. They could develop a structured therapy plan to address what might be depression.
Both professionals are dedicated to helping you live a healthier, more fulfilling life. Understanding their unique roles and approaches allows you to make an informed choice on your journey toward well-being.
Common Conditions They Address and Where They Work
One of the easiest ways to understand the difference between a counsellor and a psychologist is by looking at where they work. Their professional settings often indicate their training and the type of support they offer. This can help you decide if you need help building resilience or navigating a more persistent mental health challenge.
A counsellor's work is often embedded in everyday life settings focused on personal growth and well-being. The goal is to make support accessible where people need it most, helping them handle life's hurdles.
Psychologists, with their specialised training in assessment and complex conditions, are generally found in more clinical environments. Their work often involves a deeper exploration of mental health patterns to develop structured treatment plans.
Where You Might Meet a Counsellor
Counsellors shine in environments that prioritize proactive well-being and personal development. They help people build skills like resilience and self-compassion to manage challenges before they grow.
You’ll commonly find counsellors in settings like:
- Schools and Universities: Guiding students through academic stress, career choices, or personal anxieties.
- Corporate Wellness Programmes: Helping employees manage workplace stress, avoid burnout, and improve work-life balance.
- Community Centres: Providing accessible support for relationship problems, grief, or parenting difficulties.
- Private Practice: Offering talk therapy for clients who want to build self-esteem, improve communication, or find more happiness.
Their focus is on building your inner strengths and equipping you with practical tools for specific challenges, from stress to enhancing well-being.
Where You Are Likely to Find a Psychologist
Given their rigorous training, psychologists tend to work where a more intensive level of care is required. These settings support individuals dealing with significant mental health concerns like anxiety and depression.
Psychologists are typically based in:
- Hospitals and Mental Health Clinics: Collaborating with medical teams to treat conditions like severe anxiety or major depression.
- Private Practice: Providing specialised therapies and conducting psychological assessments for various conditions.
- Rehabilitation Centres: Assisting individuals with the psychological aspects of recovery.
- Research and Academic Institutions: Advancing the field of psychology through teaching and study.
Looking at current psychologist job opportunities can give you a practical glimpse into the breadth of their roles.
A key takeaway is that both professionals are vital to our collective well-being. A counsellor is often a great first contact for life's challenges, while a psychologist provides specialised care for more complex mental health conditions.
The professional's work setting often tells you what kind of support to expect. Whether you're aiming to boost your well-being or need help with persistent symptoms, there is someone trained to help.
Navigating Costs and Accessibility in India
Making the decision to seek mental health support is a significant step, and practical considerations like cost are important. Understanding the financial aspect can make the process feel less overwhelming. In India, there is often a difference in session fees between a counsellor and a psychologist.
This price difference is mainly due to their training and qualifications. Psychologists complete a longer, more intensive education, often including an RCI-approved M.Phil. This equips them for formal psychological assessments, which contributes to higher session fees. Budget is a valid and real-world part of choosing the right professional.
Understanding Session Fees
Session fees can vary based on experience, specialisation, and location. However, we can look at general price ranges to give you a starting point for therapy costs.
- Counsellors: A session with a qualified counsellor in India typically costs between ₹800 and ₹2,500. This often makes them an accessible option for working through issues like workplace stress or building personal resilience.
- Psychologists: With their advanced qualifications, a session with a licensed clinical psychologist usually ranges from ₹1,500 to ₹5,000. Specialists in major cities may charge more.
This difference in fees is also reflected in their earning potential, as seen in psychologist salary structures in India.
Think of therapy as a long-term investment in your mental and emotional well-being. Many professionals offer sliding scale fees based on income or discounted session packages, so don't hesitate to ask.
Accessibility and Finding the Right Fit
Cost isn't the only practical factor; availability is also key. It can sometimes be harder to find a licensed clinical psychologist due to their smaller numbers, especially outside major cities.
The good news is that the mental health landscape is improving. Platforms like DeTalks are making it easier to connect with qualified professionals across India. These services help bridge the accessibility gap, allowing you to find someone who fits your budget and understands your specific needs, whether for anxiety, depression, or personal growth.
The goal is to find support that feels right on every level. Understanding the costs and availability empowers you to make a decision that works for you, so you can focus on your well-being journey.
How to Choose the Right Professional for You
Deciding to get help is a courageous first step. The next is choosing the right person to guide you. This isn't about finding the "best" professional, but the one who is the best fit for you right now.
When you understand the difference between a counsellor and a psychologist, you can make a choice that feels right. Taking a moment to think about what you’re hoping to gain from therapy can offer incredible clarity.
Reflect on Your Current Needs
Take a gentle look at what's going on. Are you navigating a specific life event, like a stressful project at work, or is it a persistent feeling of unease?
Thinking about your challenges in these terms can help:
- Situational Hurdles: Things like managing workplace stress, grief, or adjusting to change are often well-suited for a counsellor.
- Deeper Patterns: Repeating cycles of anxiety or long-term feelings of depression that interfere with daily life may be better explored with a psychologist.
This flowchart can offer a quick visual guide for which path might make sense for your current situation.
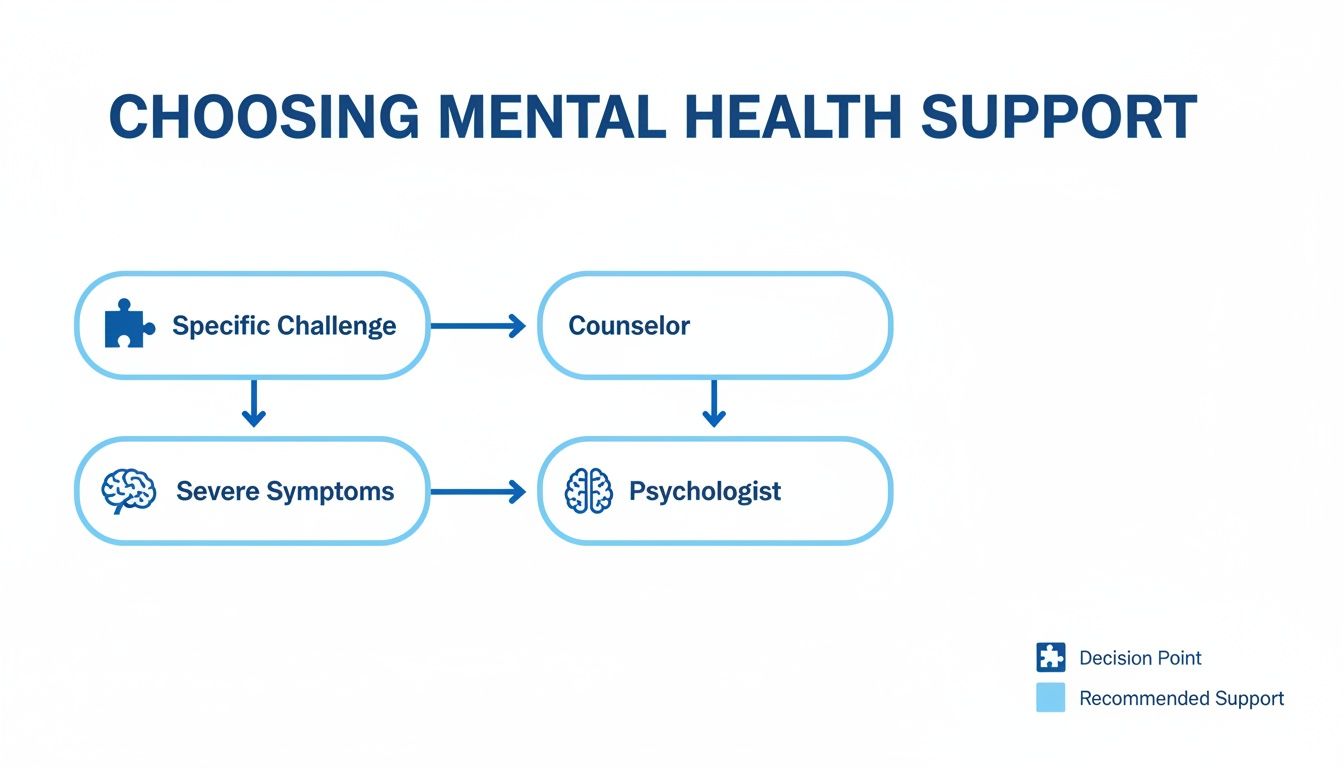
As you can see, a counsellor is a great choice for targeted support with life's challenges. A psychologist is trained to help with more severe, persistent symptoms that might have deeper roots.
Clarify Your Goals for Well-being
Now, think about what you want to achieve. Are you looking for a practical toolkit, or do you want to understand why you feel the way you do? Both are valid goals.
Consider if your aim is:
- Building Skills: If you want to learn coping mechanisms, improve communication, or build resilience, the practical approach of counselling is a great fit.
- Exploring the 'Why': If you’re curious about how your past influences your present, a psychologist’s training in human behaviour can help you connect those dots.
Your goals may change, and that's okay. Starting with a clear intention helps you find someone whose methods align with what you're trying to achieve.
The first meeting is a two-way conversation. It's your chance to see if you connect with the professional and their style. If it doesn't feel right, it's perfectly okay to look for someone else.
Questions to Ask a Potential Professional
Once you have a better sense of your needs, it's time to talk to a few professionals. The initial consultation is the perfect time to ask questions and see if their approach aligns with what you’re looking for.
Here are a few helpful questions:
- "Can you tell me a bit about your therapeutic approach?" This gives you a feel for their style—whether it's structured or more flexible.
- "What's your experience with challenges like mine?" Whether you’re dealing with anxiety, burnout, or relationship issues, it helps to know they have relevant experience.
- "What can I expect in our first few sessions together?" This helps set expectations and clarifies their process.
- "How do you and your clients track progress?" It’s useful to know if their idea of progress matches yours.
Asking these questions makes you an active partner in your well-being journey.
Your Supportive Takeaway
Choosing between a counsellor and a psychologist is a personal decision, and there is no wrong answer. Both are skilled professionals dedicated to helping you live a better, more meaningful life. The key is finding someone whose approach makes you feel safe, heard, and understood.
Taking time to reflect on what you need is a powerful act of self-care. It's the first step toward building a healthier, more resilient you.
Frequently Asked Questions
Stepping into the world of mental health support can bring up many questions. Here, we answer some common queries about counsellors and psychologists to help you move forward with confidence.
Can a Counsellor Help with Anxiety or Depression?
Yes, a counsellor can be a great support for mild to moderate anxiety or depression. Through talk therapy, they can help you build coping skills, manage daily symptoms, and improve your emotional resilience. The focus is often on your immediate challenges.
If your symptoms feel severe or persistent, a psychologist might be a better choice. Their training allows them to explore and treat more complex conditions and the underlying patterns that may be contributing to them.
Do I Need a Referral to See a Psychologist in India?
No, you do not need a referral to see a clinical psychologist in India. You can contact them directly to book an appointment. This direct access makes seeking specialised mental health care simpler and faster.
Which Professional Is Better for Workplace Stress?
For issues like burnout and workplace stress, a counsellor is often an excellent starting point. Their work is typically solution-focused, providing practical tools to manage stress, set boundaries, and improve work-life balance. They help you develop skills to navigate your professional life more effectively.
Ultimately, the right professional is the one you connect with. A strong therapeutic relationship is one of the most powerful predictors of positive outcomes, regardless of their title.
How Do I Know If I Need Formal Assessments?
You don't have to figure this out on your own. A psychologist uses formal assessments as informational tools to get a clearer picture when a more complex issue might be involved. They are not diagnostic labels.
Whether you start with a counsellor or a psychologist, they will listen to your concerns. If they believe a formal assessment could provide valuable insights, they will discuss it with you. Think of it as a way to get a more accurate map of what's happening.
Finding your way to mental well-being is a deeply personal journey, and the right guide makes all the difference. At DeTalks, we simplify the process of finding and connecting with vetted counsellors and psychologists across India. You can find the support that truly fits your needs. Take the first step by exploring our network of professionals today at https://detalks.com.